Dr. Jeremy Clark: Advancements in Prostate Cancer Detection Using Urine Biomarkers
With the acceleration of medical breakthroughs, it is easy to imagine that scientific advancements come into existence without much fuss. However, the reality is that much of the scientific discovery lies in the meticulous process itself. A journey of trial and error, hypotheses, imagination and of course, a question. We aim to shine a light on the scientific process and learn from the scientists themselves about what drives them and how they stay optimistic in a world full of dreary statistics.
An Interview with Scientist Dr. Jeremy Clark
 We recently sat down with Dr. Jeremy Clark, a lead Scientific Researcher from University East Anglia's Norwich Medical School, to learn about his research in prostate cancer (PCa) detection, the details of his recent publication, and where this important research in men’s health is heading. With prostate cancer being the second most common cancer in men, globally, this research beams optimism. Dr. Jeremy Clark is a current member of the Movember GAP1 Urine Biomarker Consortium that investigates urinary biomarkers in patients with prostate cancer. Biomarkers are increasingly becoming a critical component of personalized healthcare because of their ability to provide early disease prognostic indicators, allowing for active surveillance and treatment options. Their goal is to develop diagnostic tools to revolutionize the current methods in prostate cancer diagnosis. Dr. Clarks’ current research is funded by a Movember & Prostate Cancer UK Innovation award.
We recently sat down with Dr. Jeremy Clark, a lead Scientific Researcher from University East Anglia's Norwich Medical School, to learn about his research in prostate cancer (PCa) detection, the details of his recent publication, and where this important research in men’s health is heading. With prostate cancer being the second most common cancer in men, globally, this research beams optimism. Dr. Jeremy Clark is a current member of the Movember GAP1 Urine Biomarker Consortium that investigates urinary biomarkers in patients with prostate cancer. Biomarkers are increasingly becoming a critical component of personalized healthcare because of their ability to provide early disease prognostic indicators, allowing for active surveillance and treatment options. Their goal is to develop diagnostic tools to revolutionize the current methods in prostate cancer diagnosis. Dr. Clarks’ current research is funded by a Movember & Prostate Cancer UK Innovation award.
The History of PSA and DRE
For the past 30 years, the gold standard for prostate cancer screening has been via blood tests (prostate-specific antigen or PSA) and digital rectal examination (DRE), all of which require a hospital visit. These methods, while useful, have their limitations and criticisms. They require frequent visits with your doctor and have been reported to produce high rates of inaccurate results, creating a problem of unnecessary prostate removal surgeries in men. These unnecessary surgeries can result in life-altering consequences, such as loss of bladder control, the onset of erectile dysfunctions which can negatively impact sexual performance and more. As a result of this, scientists have investigated easier, safer and more reliable methods of prostate cancer detection.
Currently, 1 in 9 Canadian men are expected to be diagnosed with prostate cancer in their lifetime (1). The prostate-specific antigen (PSA) is a protein solely produced by the prostate gland. PSA samples are obtained from a blood test and are used to scan for signs of prostate cancer. Dr. Jeremy Clark explains that “while raised PSA levels in the blood are a sign of prostate cancer, other factors can cause PSA levels to increase as well, including urinary tract infections, age, prostate inflammation and cycling.” In fact,
"Up to 70% of men with a raised PSA are negative for cancer on tissue biopsy, producing a massive false-positive rate,” stated Dr. Clark.
In addition to the PSA test, the digital rectal examination (DRE) is also commonly used by doctors during a routine physical check to examine the prostate gland for lumps or anything unusual. Because the “prostate itself can be prone to infection and can become inflamed for a myriad of reasons, these lumps can come and go and they are not necessarily a sign of cancer,” says Dr. Clark.
In one of Dr. Jeremy Clark’s interviews, he explains that “the idea behind the urine test is as follows: The prostate lays just below the bladder, it is a secretory organ and these secretions carry cells and molecules from all over the prostate into the urethra which then get flushed out of the body on urination. If a cancer is present, tiny bits of the tumour are also carried with the secretions and can be detected in the urine.” (2)
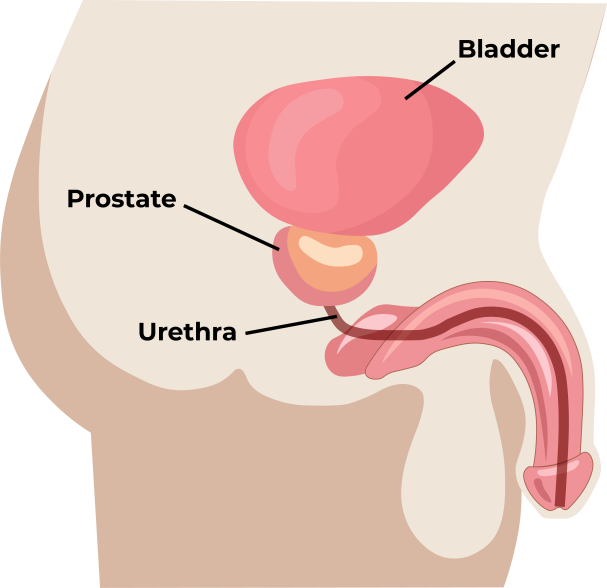 The pilot study used urine that was collected after a DRE (Digital Rectal Examination) of the prostate. During the DRE, the clinician depresses the prostate in order to squeeze secretions into the urethra. However, “when we looked at the RNA yields from 8 different clinicians, we found that there was a 10-fold difference in RNA yields between clinicians. It was clear that the variation in RNA among the clinicians was the result of the efficiency with which the prostate was depressed, which may just come down to something as simple as the length of their finger,” says Dr. Clark. With so much ambiguity with these processes, his team decided to look for another means of sample collection that could be obtained stress-free from the comfort of a patient’s home.
The pilot study used urine that was collected after a DRE (Digital Rectal Examination) of the prostate. During the DRE, the clinician depresses the prostate in order to squeeze secretions into the urethra. However, “when we looked at the RNA yields from 8 different clinicians, we found that there was a 10-fold difference in RNA yields between clinicians. It was clear that the variation in RNA among the clinicians was the result of the efficiency with which the prostate was depressed, which may just come down to something as simple as the length of their finger,” says Dr. Clark. With so much ambiguity with these processes, his team decided to look for another means of sample collection that could be obtained stress-free from the comfort of a patient’s home.
A Process of Change
In 2019, Dr. Clark’s team successfully completed a pilot study funded by Movember that described an effective home collection method of urine samples for prostate cancer detection. The scientists came across studies that suggested the prostate gland is continuously secreting into the urethra. This gave them the idea to collect urine from the patient first thing in the morning since the prostate would have been producing secretions throughout the night. Indeed, this proved to be the case as good yields of biomarkers were detected in these ‘morning’ samples. The new collection kit contains two tubes, one for the morning sample, and one for a second urine sample collected one hour later which should provide the most consistent amount of secretions in the urethra. “The urine test is a way of holistically looking at the whole of the prostate in one go,” explains Dr. Clark. He continues by explaining how urine provides a non-invasive way to examine the health status of the patient’s prostate and establish the progression or aggression of the disease with relative ease.
However, for the pilot study, RNA had to be extracted from each urine sample within 3 hours, otherwise the RNA disappeared. Dr. Jeremy Clark knew that in order to put the Home Collection system into place, a urine preservative was needed to stabilize the RNA in the urine and maintain sample integrity.
Stabilizing Urinary RNA
 Without a stabilizing buffer, urinary RNA becomes fragmented and RNA yields rapidly decrease, affecting the ability to screen for biomarkers. They reasoned that by using an efficient urine preservative that stabilizes RNA (and microRNA) at room temperature, an effective way to study urinary biomarkers for prostate cancer detection could be achieved. Samples can be collected and preserved all in one go, without pressure and without the need for immediate processing. The Norgen preservative (Cat. 18118, 18122, 18113, 18126, 18129) was found to fulfill all of these needs and became the bedrock of the Home Collection system.
Without a stabilizing buffer, urinary RNA becomes fragmented and RNA yields rapidly decrease, affecting the ability to screen for biomarkers. They reasoned that by using an efficient urine preservative that stabilizes RNA (and microRNA) at room temperature, an effective way to study urinary biomarkers for prostate cancer detection could be achieved. Samples can be collected and preserved all in one go, without pressure and without the need for immediate processing. The Norgen preservative (Cat. 18118, 18122, 18113, 18126, 18129) was found to fulfill all of these needs and became the bedrock of the Home Collection system.
The researchers from UEA's Norwich Medical School found that urine samples taken at home with preservative contained higher levels of cancer biomarkers than samples collected after a DRE. With this information, they put together an effective Home Collection system whereby urine samples are shipped by the patient back to the laboratory for analysis and prostate cancer detection. The findings in this research are auspicious.
NORBLOG
Want to hear more from Norgen?
Join over 10,000 scientists, bioinformaticians, and researchers who receive our exclusive deals, industry updates, and more, directly to their inbox.
For a limited time, subscribe and SAVE 10% on your next purchase!
SIGN UP
Since the results of the pilot study in 2019, Dr. Clark explains how the team has moved on to the validation phase for the Home-Urine Collection Test, funded by a Movember & Prostate Cancer UK Innovation award. This phase involves around 1,500 men at selected sites worldwide and includes men with a raised PSA and thus a suspicion of prostate cancer as well as men known to have low-risk prostate cancer disease. Results are expected in the next 2-3 years.
Future Implications of Urine Biomarkers
We asked Dr. Jeremy Clark some questions about what the future of this research looks like and advice for future scientists.
What would you describe as the future implications of this research?
“Right now in the UK, when a man turns 60 they receive a sample tube in the mail to collect a fecal sample, which is then returned to a lab to check for bowel cancer. The same sort of thing could work well for prostate cancer with a urine sample.” This method “will enable clinics to screen men for prostate cancer with a much higher consistency rate than PSA, and the whole test is easily adaptable for bladder and kidney cancer as well.” - Dr.Clark
If you could offer advice to a young, aspiring scientist, what would it be?
“[Science]…It’s like a detective story, there are lots of red herrings and false alleyways, and it’s the excitement of all that. It’s the results that don’t agree with your theory that are the important ones. These make you stop and rethink, find another theory of explanation. That is the really exciting part. You may go looking for one thing, but you find something much more exciting along the way.” - Dr. Clark
Dr. Jeremy Clark and his team at Norwich Medical are currently researching DNA methylation in urine. You can read the results of their publication here.
Research Funding
 This research was funded by the Movember Foundation GAP1 Urine Biomarker project, The Masonic Charitable Foundation, The Bob Champion Cancer Trust, the King family, The Andy Ripley Memorial Fund and the Stephen Hargrave Trust
This research was funded by the Movember Foundation GAP1 Urine Biomarker project, The Masonic Charitable Foundation, The Bob Champion Cancer Trust, the King family, The Andy Ripley Memorial Fund and the Stephen Hargrave Trust
If you would like to support this important work, consider making a donation to the Movember Foundation.
Thank you Dr. Clark for speaking with the Norgen team and sharing your insight on this incredible work!
References
-
Canadian Cancer Society. (2020). Prostate Cancer Statistics - Canadian Cancer Society. Retrieved April 30, 2021, from https://www.cancer.ca/en/cancer-information/cancer-type/prostate/statistics/?region=on.
Benz, M. (2019, December 2). Home Urine Test May Predict Aggressive Prostate Cancer Prior to Biopsy. MedicalResearchcom. https://medicalresearch.com/cancer-_-oncology/prostate-cancer/home-urine-test-may-predict-aggressive-prostate-cancer-prior-to-biopsy/52336/.