Renal inflammatory pathway mediation by miRNA: isolation and quantification of miR-103a-3p
RNA isolation and quantification of miRNAs are gaining significance as promising methods in cancer biomarker discovery. Establishing standardized protocols for collection, sample storage conditions, and the use of exogenous and endogenous controls for normalization are all critical aspects to reliably quantify miRNA levels which can be further implemented in a clinical laboratory setting.
Quilun et al. at the University of Georgia, Atlanta have determined that circulating miR-103a-3p levels are higher when Angiotensin II (Ang II) is present, which suppresses the expression of sucrose non-fermentable-related serine/threonine-protein kinase (SNRK) in glomerular endothelial cells and results in overactivation of NF-κB/p65. Ultimately, these processes give rise to inflammatory injury and fibrosis1.
Ang II is elevated in instances of hypertension-induced renal injury and fibrosis2. The mechanism by which this hormone induces renal dysfunction is still unclear but there are strong correlations between circulating miRNA dependent Ang II function and kidney diseases.
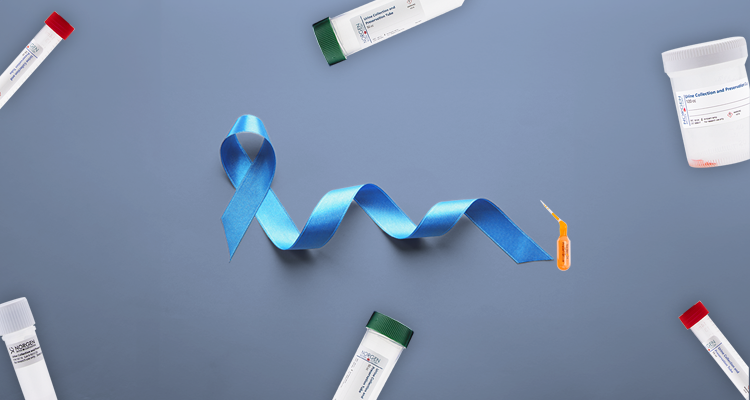
The purification kit used to purify the total urinary microRNAs was Norgen's Urine MicroRNA Purification Kit (Cat. #29000). Total circulating microRNAs were isolated using miRNeasy Serum/Plasma Kit (QIAGEN, Germany). Total microRNAs from kidney tissues and cells were purified using mirVana miRNA Isolation Kit (Thermo Fisher Scientific, Waltham, MA).
Data was assessed through qRT-PCR for endogenous miRNA and for cel-miR-39 spike-in. In order to provide a correlation between Ang II-induced renal injury and circulating microRNAs, miR-103a-3p levels in human urine and blood samples were tested in both normotensive healthy and hypertensive nephropathy patients (Fig. 1). Quilun et al. found that increased levels of Ang II led to an increase of the miRNA, downregulating SNRK in renal endothelial cells, with subsequent overactivation of NF-κB/p65 giving rise to renal injury.
NORBLOG
Want to hear more from Norgen?
Join over 10,000 scientists, bioinformaticians, and researchers who receive our exclusive deals, industry updates, and more, directly to their inbox.
For a limited time, subscribe and SAVE 10% on your next purchase!
SIGN UP
It is evident that Ang II causes renal injury and fibrosis through signalling mechanisms related to increased levels of circulating miR-103a-3p, endothelial SNRK, and p65. Unique patterns of aberrant miRNA expression may serve as molecular biomarkers for tumour diagnosis, prognosis of disease-specific outcomes, and prediction of therapeutic responses. Targeting the levels of these signals will help regulate renal injuries; thus, it is critical to use precise miRNA extraction and quantification methods for detection.

Figure 1. Circulating miR-103a-3p is upregulated in hypertensive nephropathy patients and AngII-treated mice. a–c Albumin/creatinine ratio (ACR) (a), serum miR-103a-3p levels (b), and ratio for urinary miR-103a-3p levels to the volume of 24 h urine (c) of hypertensive nephropathy (HN) patients (n = 31) and healthy controls (n = 18). d, e Correlation between ACR and the ratio for urinary miR-103a-3p levels to the volume of 24 h urine (d) or serum miR-103a-3p levels (e) in healthy individuals and HN patients. f–k Albumin excretion rates (f), ACR (g), systolic blood pressure (SBP) (h), ratio for urinary miR-103a-3p levels to the volume of 24 h urine (i), and serum miR-103a-3p levels (j) in wild-type mice (n = 8) infused with vehicle (Veh) or AngII (0.2 or 1 mg kg−1 d−1) for 4 weeks. (k) Correlation between circulating miR-103a-3p levels and ACR in vehicle- or AngII-infused mice.
-
Lu, Q., Ma, Z., Ding, Y., Bedarida, T., Chen, L., Xie, Z., … & Zou, M. H. (2019). Circulating miR-103a-3p contributes to angiotensin II-induced renal inflammation and fibrosis via a SNRK/NF-κB/p65 regulatory axis. Nature communications, 10(1), 2145.
-
Kim, S., Ohta, K., Hamaguchi, A., Omura, T., Yukimura, T., Miura, K., … & Chatani, F. (1994). Role of angiotensin II in renal injury of deoxycorticosterone acetate-salt hypertensive rats. Hypertension, 24(2), 195-204.