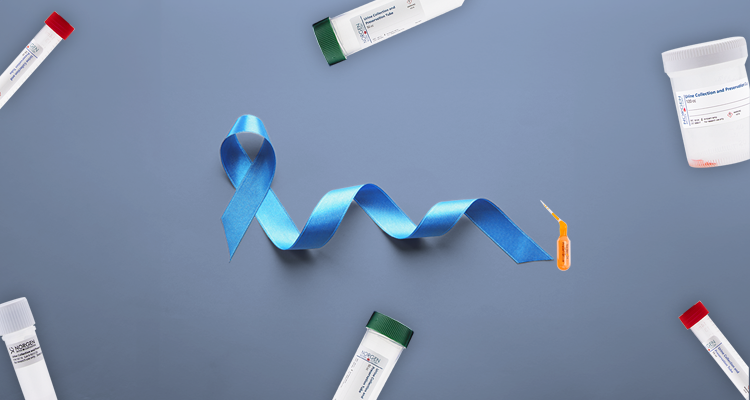
Innovative Discovery for SARS-CoV-2 Sample Collection
In this blog, you are going to learn about different viable sample types for the detection of SARS-CoV-2 in infected individuals.
This blog includes data collected from real life experiments using live samples of the SARS-CoV-2 virus, proving that saliva can be used for detection and diagnostic purposes.
If you don’t want to get your brain tickled with a nasopharyngeal swab when testing for COVID-19, keep on reading!
Due to the global COVID-19 pandemic, it seems more nasal cavities are being picked, or swabbed, than ever before. Sample collection for the virus has been predominantly collected through nasopharyngeal swabs, however, due to global shortages in swabs, alternatives needed to be explored. The preliminary work by Wyllie et al. (2020 Preprint) has found that saliva samples experience less variability over time and provide more viral RNA copies. Additionally, a new preliminary report from Kojima et al. (2020 Preprint) found that self-collected saliva and nasopharyngeal swabs offer similar or possibly better capacity to collect viral RNA. In other words, there is no more need to climb through the nasal cavity to look for SARS-CoV-2.
Work by Kojima et al. (2020 Preprint) included SARS-CoV-2 infected individuals and non-infected individuals. Samples were collected through three methods: clinically-supervised self-collected saliva and nasal swabs, unsupervised self-collected saliva, and clinically-collected nasopharyngeal swabs. Each sample was collected in nucleic acid preservative and then processed through Norgen Biotek’s Total RNA Purification 96-Well Kit. The kit allowed for automated high-quality RNA purification on the Tecan Resolvex A200, and the authors used a modified CDC-primer/probe assay to quantify SARS-CoV-2 copies. The results were compelling!

NORBLOG
Want to hear more from Norgen?
Join over 10,000 scientists, bioinformaticians, and researchers who receive our exclusive deals, industry updates, and more, directly to their inbox.
For a limited time, subscribe and SAVE 10% on your next purchase!
SIGN UP
Figure 1. SARS-CoV-2 titers are higher in the saliva than nasopharyngeal swabs from hospital inpatients. (a) All positive nasopharyngeal swabs (n = 46) and saliva samples (n = 39) were compared by Mann-Whitney test (p < 0.05). Bars represent the the median and 95% Cl. Our assay detection limits of SARS-CoV-2 using the US CDC “N1” assay is at a cycle threshold 38, which corresponds to 5,610 virus copies/mL of sample (shown as dotted line and grey area). (b) Patient matched samples (n = 38), represented by the connecting lines, were compared by a Wilcoxon test test (p < 0.05). (c) Patient matched samples (n = 38) are also represented on a scatter plot. All of the data used to generate this figure, including the raw cycle thresholds, can be found in Supplementary Data 1. Extended Data Fig. 1 shows the correlation between US CDC assay “N1” and “N2” results.
Kojima et al. (2020 Preprint) found that detection of SARS-CoV-2 from supervised self-collected saliva samples performed even better than clinically-collected nasopharyngeal samples (Figure 1). The eager long lines to get a six inch swab inserted up the nose could be a thing of the past! Now patients can collect their own saliva sample to test for SARS-CoV-2, bypassing the nasopharyngeal swab and more importantly, reducing the likelihood of viral transmission.
It is crucial in these uncertain times to find new, innovative and safer ways to collect samples. Norgen Biotek’s solution, Saliva RNA Collection and Preservation Devices, enables a physically distanced sample collection, whether collected at home or at a healthcare facility. Additionally, our Saliva/Swab RNA Purification Kit offers an alternative to purify high quality total RNA, including viral RNA, without any bias where neither RNA carrier nor phenol-chloroform are required.For more information on our complete SARS-CoV-2 workflow, please visit the product pages below or contact us at info@norgenbiotek.com.

| Description | Size | Cat. No. | ||
|---|---|---|---|---|
|
50 units | RU53800 or Dx53800 | ||
| Total Nucleic Acid Preservation Tubes | 50 units | 69200 or Dx69200 | ||
| Saliva/Swab RNA Purification Kit | 50 preps | 69100 or Dx69100 | ||
| Saliva/Swab RNA Purification Kit 96-Well Kit | 2 x 96-Well Plates | 69300 or Dx69300 | ||
| COVID-19 TaqMan RT-PCR Kit (E/RdRP genes) | 500 rxns | TM67200 | ||
| 2019-nCoV TaqMan RT-PCR Kit | 500 rxns | TM67120 |
For more information about how Saliva is a viable sample type for SARS-CoV-2 detection, check out our previous blog here.
- Azzi, L., Carcano, G., Gianfagna, F., Grossi, P., Gasperina, D. D., Genoni, A., Fasano, M., Sessa, F., Tettamanti, L., Carinci, F., Maurino, V., Rossi, A., Tagliabue, A., & Baj, A. (2020). Saliva is a reliable tool to detect SARS-CoV-2. Journal of Infection, 81(1), e45–e50. DOI: 10.1016/j.jinf.2020.04.005
- Kojima, N., Turner, F., Slepnev, V., Bacelar, A., Deming, L., Kodeboyina, S., & Klausner, J. D. (2020). Self-Collected Oral Fluid and Nasal Swabs Demonstrate Comparable Sensitivity to Clinician Collected Nasopharyngeal Swabs for Covid-19 Detection [Preprint]. DOI: 10.1101/2020.04.11.20062372
- Wyllie, A. L., Fournier, J., Casanovas-Massana, A., Campbell, M., Tokuyama, M., Vijayakumar, P., Geng, B., Muenker, M. C., Moore, A. J., Vogels, C. B. F., Petrone, M. E., Ott, I. M., Lu, P., Lu-Culligan, A., Klein, J., Venkataraman, A., Earnest, R., Simonov, M., Datta, R., Handoko, R., Naushad, N., Sewanan, L. R., Valdez, J., White, E. B., Lapidus, S., Kalinich, C. C., Jiang, X., Kim, D. J., Kudo, E., Linehan, M., Mao, T., Moriyama, M., Oh, J. E., Park, A., Silva, J., Song, E., Takahashi, T., Taura, M., Weizman, O.-E., Wong, P., Yang, Y., Bermejo, S., Odio, C., Omer, S. B., Dela Cruz, C. S., Farhadian, S., Martinello, R. A., Iwasaki, A., Grubaugh, N. D., & Ko, A. I. (2020). Saliva is more sensitive for SARS-CoV-2 detection in COVID-19 patients than nasopharyngeal swabs [Preprint]. DOI: 10.1101/2020.04.16.20067835