As the 2022-2023 flu season begins, hospitals across North America have reported increased cases and severity compared to past years. Influenza typically peaks between December and January but has seemingly arrived early this year, with over 880,000 cases in the US already, according to CDC estimates.1 Based on the number of lab-confirmed cases, vaccination counts, hospitalizations and deaths, experts worry this could be the worst flu season in 13 years.1
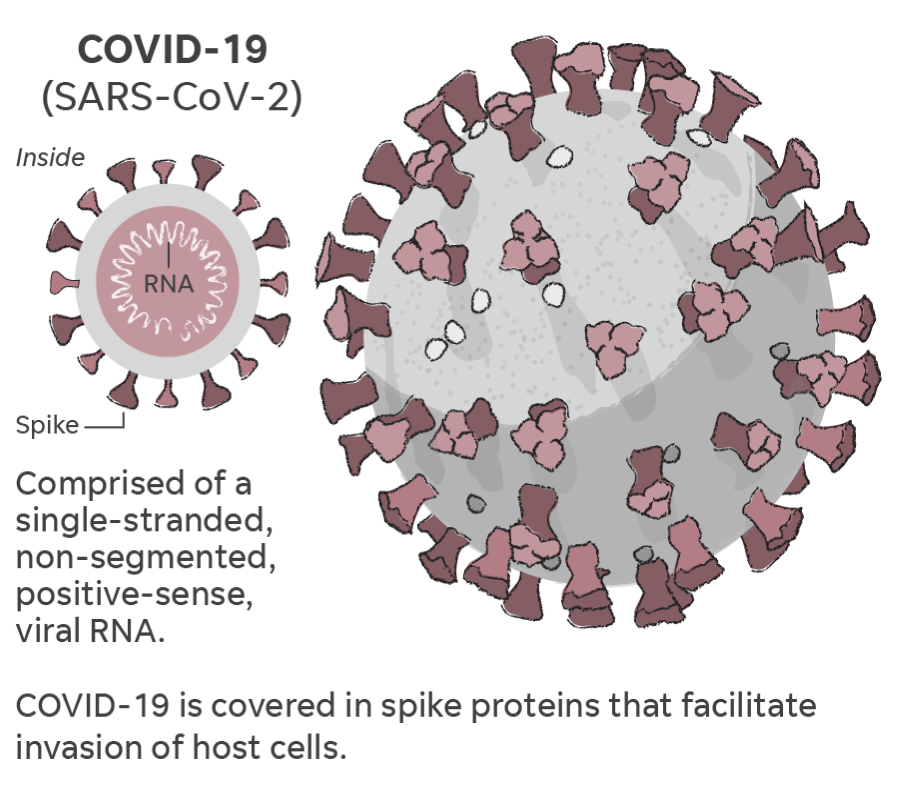
In addition, as temperatures continue dropping and in-person events move indoors, COVID-19 cases are expected to increase, which adds another layer of concern for healthcare professionals.1 With many of the presenting, short-term symptoms of Influenza being similar, if not identical, to those caused by COVID-19, molecular testing for not only one, but both, will be essential this flu season to ensure proper treatment and avoid over-straining our delicate healthcare systems further.2,3
The Flu:
 How many times have you heard someone say “Oh, it’s just the flu” when they have come down with something? Though it may be unpleasant, most people overcome the flu after a few days of bed rest and are usually none the worse for wear. However, lower respiratory infections, including the flu, are the fourth leading cause of death world-wide, responsible for 6% of all mortality with 2.6 million deaths in 2019.3 Lower income countries are by far hit the hardest by communicable disease, with lower respiratory infection being the second leading killer.3 Even in high income countries, lower respiratory infections are the 6th leading cause of death, which indicates it's severity.3,4 During the flu season of 2018-2019, prior to the pandemic, there were approximately 34.2 thousand deaths, 491 thousand hospitalizations, 16.5 million medical visits, and 35.5 million cases of influenza in the United States alone.5 This means that more than one out of every ten people in the USA reported having the flu during the 2018-2019 season. Keep in mind, the total number of infections is derived from the number of reported medical visits and is therefore likely lower than the actual number of infections.3
How many times have you heard someone say “Oh, it’s just the flu” when they have come down with something? Though it may be unpleasant, most people overcome the flu after a few days of bed rest and are usually none the worse for wear. However, lower respiratory infections, including the flu, are the fourth leading cause of death world-wide, responsible for 6% of all mortality with 2.6 million deaths in 2019.3 Lower income countries are by far hit the hardest by communicable disease, with lower respiratory infection being the second leading killer.3 Even in high income countries, lower respiratory infections are the 6th leading cause of death, which indicates it's severity.3,4 During the flu season of 2018-2019, prior to the pandemic, there were approximately 34.2 thousand deaths, 491 thousand hospitalizations, 16.5 million medical visits, and 35.5 million cases of influenza in the United States alone.5 This means that more than one out of every ten people in the USA reported having the flu during the 2018-2019 season. Keep in mind, the total number of infections is derived from the number of reported medical visits and is therefore likely lower than the actual number of infections.3
Want to hear more from Norgen?
Join over 10,000 scientists, bioinformaticians, and researchers who receive our exclusive deals, industry updates, and more, directly to their inbox.
For a limited time, subscribe and SAVE 10% on your next purchase!
SIGN UP
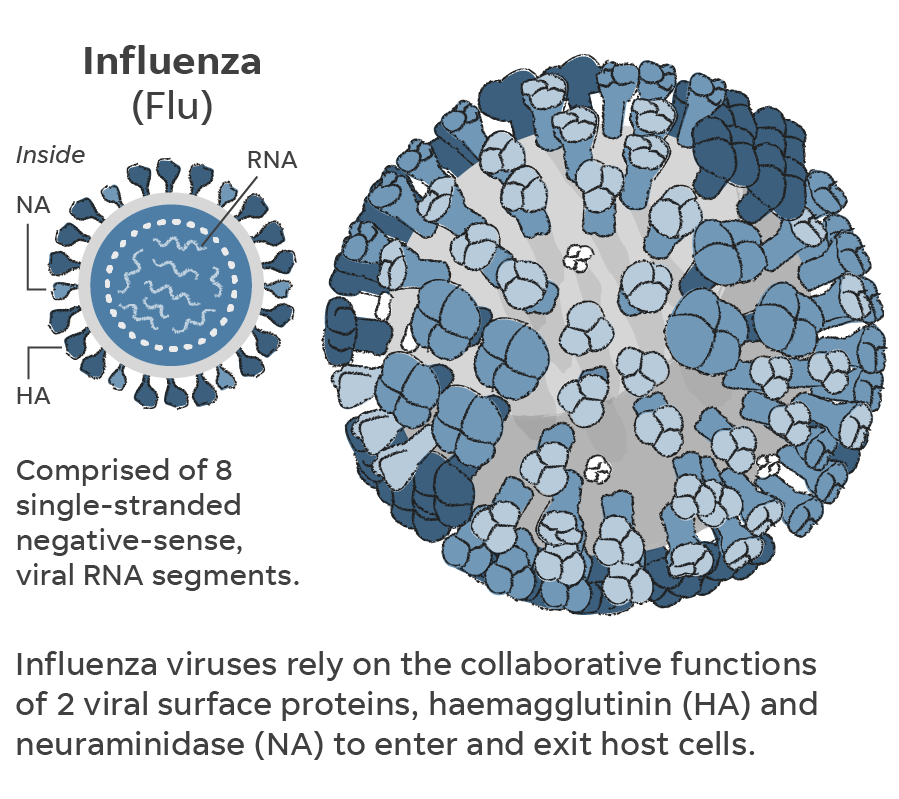
There are currently four common strains of the flu, conveniently named Influenza A, Influenza B, Influenza C and Influenza D.6 The first two strains, A and B, are the ones responsible for the seasonal outbreaks every year and are thus the ones vaccinated against. Influenza A is the more complex of the two, having multiple sub-strains based on which permutation of two surface antigens (hemagglutinin and neuraminidase) are present.6 Many of you will be familiar with a particularly virulent strain of influenza that made world wide news several years ago under the identifier H1N1. Due to its high infectivity and more severe symptoms, this particular strain, alongside another, H3N2, are present in most of the commonly available vaccines alongside Influenza B. 6
COVID and The Flu:
https://www.usatoday.com/in-depth/graphics/2020/10/13/flu-covid-19-how-tell-difference-seasonal-influenza/5880649002/.
 While both COVID and influenza may share many of the same symptoms, they are not the same disease and thus require different treatment procedures. As such, diagnosing whether a patient has one, the other, or both is critical to ensuring they receive proper care. If a patient has the flu, antiviral agents have been developed that can help treat it and reduce the severity and duration of the symptoms.1 However, these therapies will not work for a patient who has COVID and would be a waste of time and resources while the patient remains untreated. Co-infection with both viruses leads to much more severe symptoms as it increases the viral load within your body.7 This leads to more lung tissue damage, making it easier for the COVID virus to infiltrate the host cells.7 Thus, patients with both infectious agents present in their system should likely be triaged higher than those with only one if all other considerations are equal. Fortunately, molecular tests are available that can diagnose a patient with COVID as well as the two previously mentioned strains of influenza (A and B). These tests make use of powerful qPCR technology and are known collectively as multiplex PCR testing.2 By testing for COVID and influenza A and B from one sample, both time spent and the amount of sample needed can be reduced, thereby decreasing response time.2 When a patient is critically ill, this can make all the difference in terms of final outcome.
While both COVID and influenza may share many of the same symptoms, they are not the same disease and thus require different treatment procedures. As such, diagnosing whether a patient has one, the other, or both is critical to ensuring they receive proper care. If a patient has the flu, antiviral agents have been developed that can help treat it and reduce the severity and duration of the symptoms.1 However, these therapies will not work for a patient who has COVID and would be a waste of time and resources while the patient remains untreated. Co-infection with both viruses leads to much more severe symptoms as it increases the viral load within your body.7 This leads to more lung tissue damage, making it easier for the COVID virus to infiltrate the host cells.7 Thus, patients with both infectious agents present in their system should likely be triaged higher than those with only one if all other considerations are equal. Fortunately, molecular tests are available that can diagnose a patient with COVID as well as the two previously mentioned strains of influenza (A and B). These tests make use of powerful qPCR technology and are known collectively as multiplex PCR testing.2 By testing for COVID and influenza A and B from one sample, both time spent and the amount of sample needed can be reduced, thereby decreasing response time.2 When a patient is critically ill, this can make all the difference in terms of final outcome.
COVID-19 is still a threat and likely will be for a long while to come. It has put a massive strain on healthcare systems around the world and an even larger strain on the bodies of its victims. When combined with what is likely going to be a particularly harsh flu season, the results may be catastrophic if we are not properly prepared. Consistent testing will be key to ensure proper triage and treatment in the coming months. If you are interested in multiplex PCR testing, check out our COVID-19/Influenza (A & B) TaqMan RT-PCR Kit.