Colorectal cancer (CRC), also known as bowel cancer, is one of the most common cancers worldwide. Affecting the colon or rectum, it often begins as noncancerous growths called polyps, which can become cancerous over time. Early detection and treatment are crucial to improving survival rates. This comprehensive guide will explore colorectal cancer's symptoms, causes, risk factors, diagnostic methods, and treatments.
What is Colorectal Cancer?
Colorectal cancer includes two types of cancer: colon cancer, which affects the largest part of the intestine, and rectal cancer, which impacts the rectum, the final portion of the large intestine. CRC typically develops slowly, often taking months or even years to spread to other parts of the body. Because of this gradual progression, early detection significantly increases the chances of successful treatment. However, a major challenge with CRC is that symptoms are often minimal or absent in its early stages, emphasizing the importance of routine screenings. Gaining a clear understanding of this disease is a critical first step in taking proactive measures to reduce its impact.
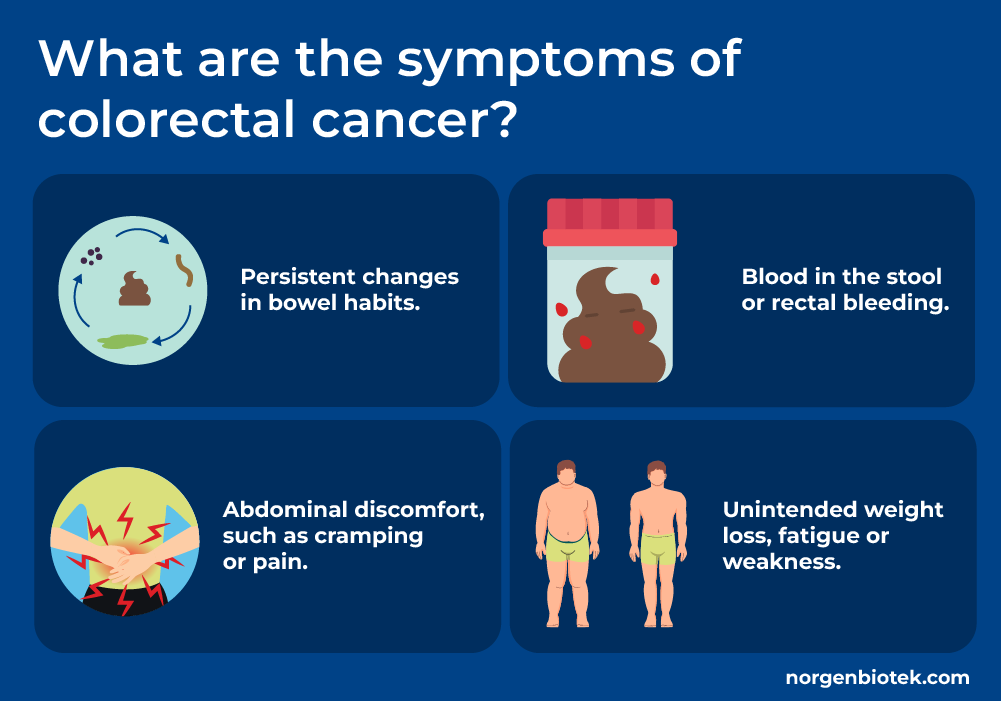
Common Symptoms of Colorectal Cancer
Generally patients in early stages of CRC show no symptoms or have minor symptoms. In later stages of colorectal cancer symptoms may vary depending on the tumor's size and location but often include:
Persistent changes in bowel habits
The bowel habits vary between individuals and “normal” habits are different among people. Constipation, diarrhea, changes in size, shape and consistency of stool are some examples of bowel habits.
Blood in the stool or rectal bleeding
Polyps and tumors can bleed for multiple reasons including, disruption of blood vessels in the lining of intestine, ulceration, inflammation and irritation of surrounding tissue, and physical damage by bowel movement due to blockage.
Abdominal discomfort, such as cramping or pain
This may include bloating and a persistent feeling of fullness. The location of the discomfort often varies depending on the tumor's position. In women, these symptoms can resemble menstrual cramps, making them easy to overlook.
Unintended weight loss, Fatigue or weakness
A large amount of weight loss (more than 10 pounds) in a short period of time accompanied by loss of energy is the symptom of many different cancers and should be addressed immediately.
If you experience any of these symptoms, consult a healthcare professional promptly.
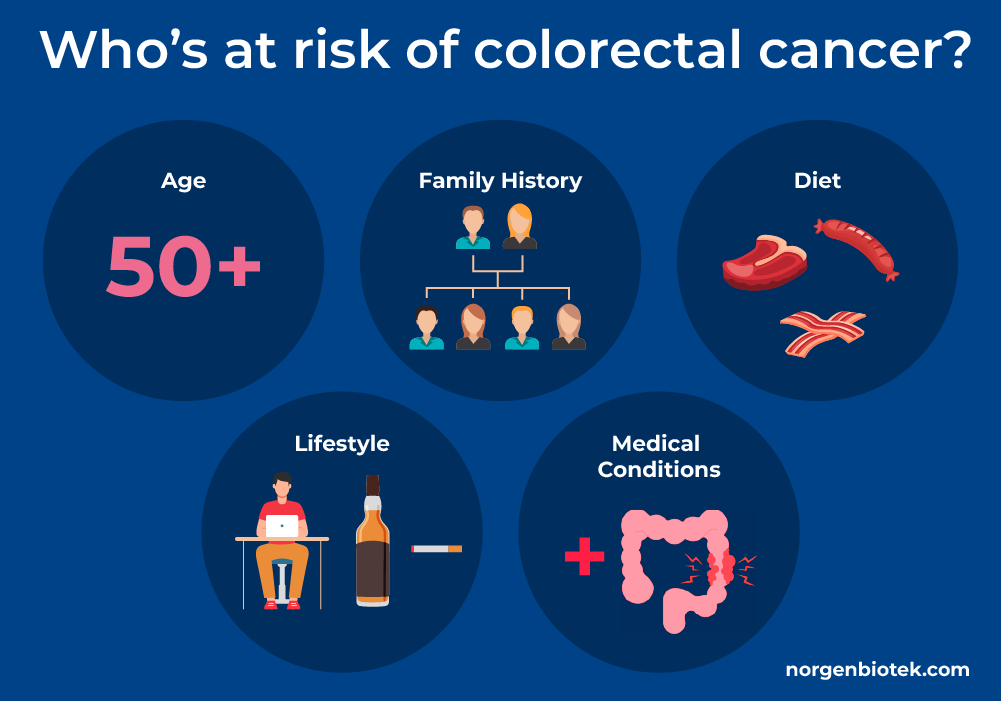
Understanding the Causes and Risk Factors of CRC
Colorectal cancer arises from genetic mutations that trigger abnormal cell growth. While some mutations are hereditary, others are influenced by environmental or lifestyle factors.
Want to hear more from Norgen?
Join over 10,000 scientists, bioinformaticians, and researchers who receive our exclusive deals, industry updates, and more, directly to their inbox.
For a limited time, subscribe and SAVE 10% on your next purchase!
SIGN UP
Key Risk Factors
Age: Colorectal cancer predominantly affects those over 50, but concerning trends show a 1-2% annual increase in cases among younger adults since the mid-1990s.21, 22 Alarmingly, rates among people under 50 have surged by 2.4% yearly, with mortality rising 1% annually.23
Family History: Having a family history of colorectal cancer significantly raises the risk, particularly if a first-degree relative was diagnosed with CRC. Around 1 in 10 cases are linked to family history, highlighting the importance of early and frequent screenings for individuals with elevated risk.21, 24
Diet: A diet high in red and processed meats significantly increases the risk of colorectal cancer, while fiber-rich foods like whole grains can reduce that risk. Studies also show that consuming 300 milligrams of calcium daily, equivalent to a large glass of milk, may lower the risk by 17 percent.25, 26
Lifestyle: Certain lifestyle habits significantly influence colorectal cancer risk. Prolonged sitting increases the risk of colon cancer by 28–44%, and behaviors like smoking and alcohol consumption also contribute to higher risks. Alcohol, in particular, is associated with several types of cancer, including colorectal cancer.27, 28
Medical Conditions: People with chronic inflammatory bowel diseases, such as Crohn's disease or ulcerative colitis, face a significantly elevated risk of colorectal cancer. Studies show that long-term inflammation in the colon substantially increases this risk, emphasizing the need for regular screenings.29
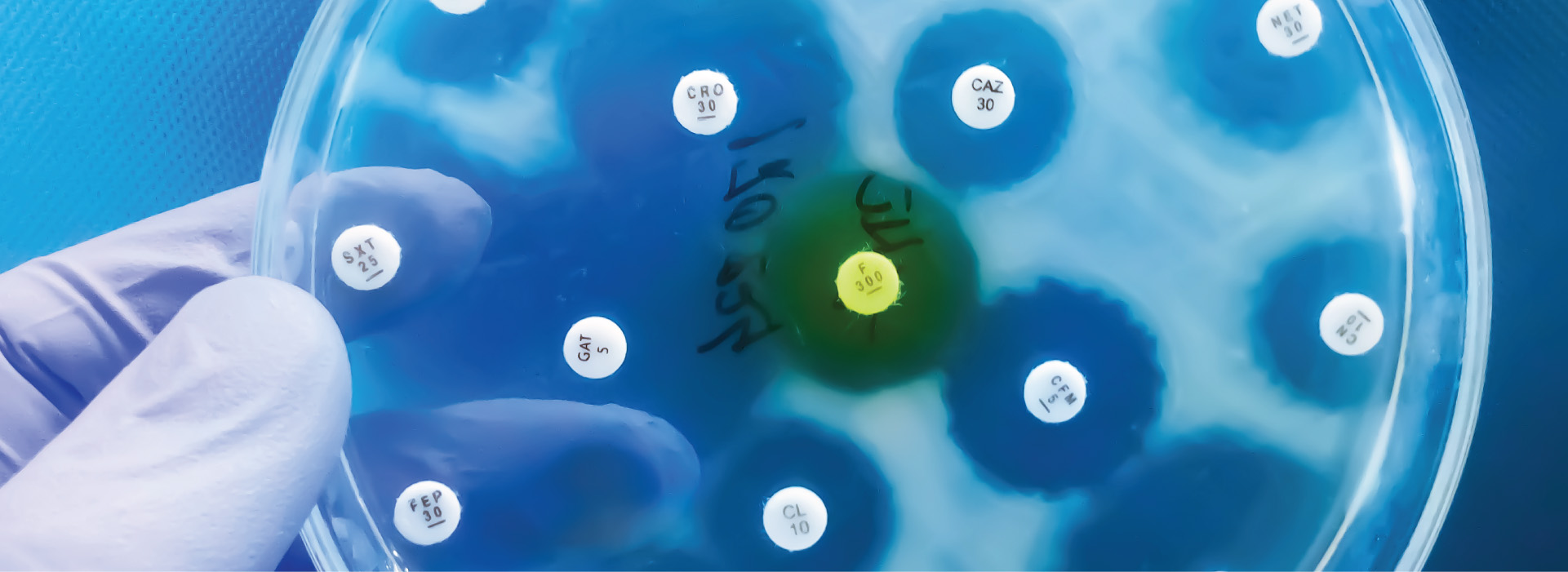
How is Colorectal Cancer Diagnosed?
Colorectal cancer (CRC) is diagnosed through a combination of screening tests, diagnostic procedures, and laboratory analyses. Early detection plays a crucial role in improving outcomes and survival rates. Based on patients' medical history, physical exam, and CRC screening test results, they will be asked to perform the following tests and procedures to rule out CRC.
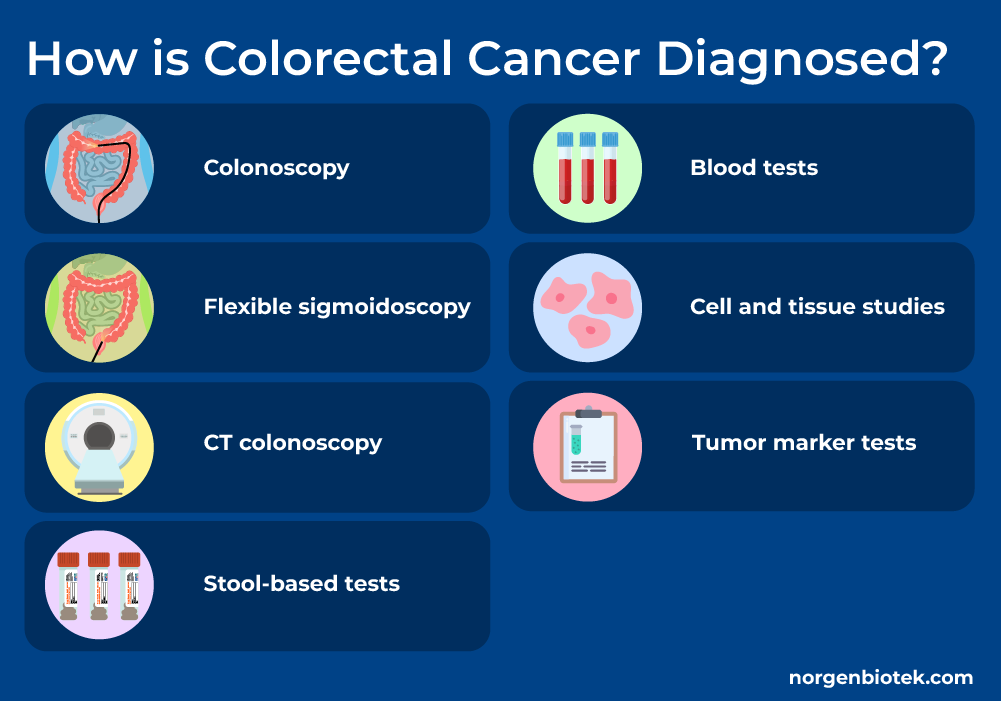
Colonoscopy
The gold standard for detecting polyps or cancer. A flexible tube with a camera examines the entire colon and rectum. Biopsy or removal of polyps can be done during a colonoscopy.
Flexible Sigmoidoscopy
It is similar to colonoscopy but less invasive. It only examines the lower portion of the colon and the rectum.
CT Colonoscopy
A minimally invasive procedure to visualize the colon that requires no sedation. This technique examines the large intestine for polyps, tumors, and other abnormalities. It utilizes computed tomography (CT) scanning technology to produce detailed, high-resolution, 3D images of the colon and rectum.
Stool-Based Tests
Presence of blood in stool could be an indication of CRC. Fecal occult blood tests (FOBT) and fecal immunochemical tests (FIT) can be used to detect blood in stool samples.
Blood Tests
Blood tests can not be used independently to diagnose CRC. However these tests provide an insight to someone's overall health and detect issues that might be connected to the presence of cancer. Individuals suspected of having CRC usually will be tested for full blood count, liver function, and kidney function.
Cell and Tissue Studies
After the presence of a tumor is detected, investigation of the presence of certain mutations in the tumor cells can determine the best treatment and therapy option for the individual.
Norgen Biotek provides researchers with a variety of techniques for DNA and RNA isolation from cell and tissue samples.
Tumor marker Tests
Advanced methods, such as RNA or DNA analysis, identify genetic markers of cancer and aid in early tumor detection. Tumor markers are found in blood, tissues or fluids removed from the body. An abnormal amount of a tumour marker may indicate that a person has colorectal cancer. Tumour marker tests are also used to check your response to cancer treatment.
Norgen Biotek provides state-of-the-art solutions for liquid biopsy biomarker testing, ensuring precise and reliable diagnostics.
Stages of Colorectal Cancer
Understanding the stages of colorectal cancer is critical for determining the most effective treatment approach.
Stage 0 colorectal cancer
At this earliest stage, abnormal cells are present only in the innermost lining of the colon or rectum and have not spread to nearby tissues. This stage is also known as carcinoma in situ.
Stage 1 colorectal cancer
Cancer has spread into the deeper layers of the colon or rectum but has not reached the lymph nodes.30 Approximately 34.8% of colorectal cancers are diagnosed at this localized stage, with a 5-year relative survival rate of 91.1%.31
Stage 2 (A-C) colorectal cancer
At this stage, cancer has grown through the wall of the colon or rectum but hasn't spread to nearby lymph nodes. Approximately 75% of people with stage II A colon cancer will be cancer-free five years after treatment without additional chemotherapy, though 25% will experience recurrence.33
Stage 3 (A-C) colorectal cancer
At this stage, colorectal cancer has spread to nearby lymph nodes but has not metastasized to distant organs. According to the SEER Training Modules, the 5-year survival rate for stage III colorectal cancer ranges from 35% to 55%, depending on the extent of lymph node involvement.34
Stage 4 (A-C) colorectal cancer
At this advanced stage, colorectal cancer has metastasized to distant organs, most commonly the liver or lungs. The five-year relative survival rate is approximately 13%, but advancements in treatment are improving outcomes for some patients.35 For those whose cancer has spread only to the liver or lungs, surgery may offer a chance of cure, and more patients with stage IV cancer are living beyond two years.36
Treatment Options for Colorectal Cancer
Surgery
Polypectomy: Removes polyps during a colonoscopy.
Colectomy: Removes part or all of the colon containing cancer.
Surgery is most effective at an early stage and when cancer has not spread to other parts of the body.
Chemotherapy
Uses strong chemical substances to kill cancer cells. This is a systemic treatment and affects cells throughout the body.
Radiation Therapy
High-energy rays are used to target and destroy cancer cells, particularly in cases of rectal cancer. These rays work by disrupting the DNA within the cells, effectively limiting their ability to divide and replicate. While radiation affects all cells, it is especially damaging to rapidly dividing cells, such as cancer cells.
Targeted Therapy
Targeted therapies are designed to focus on specific characteristics of cancer cells, inhibiting their growth while causing minimal harm to healthy cells. Examples include drugs that target epidermal growth factor receptors (EGFR), such as Panitumumab; drugs that target vascular endothelial growth factor (VEGF), such as Bevacizumab; and drugs like Encorafenib, which target cancer cells with mutations in the BRAF gene.
Immunotherapy
Use of immune checkpoint inhibitors to enable the immune system to fight cancer cells more effectively. Immunotherapy is only effective in a subset of patients that have specific genetic changes in their tumours such as, high microsatellite instability (MSI-H) or mutations in one of the mismatch repair (MMR) genes.
How to Prevent Colorectal Cancer
Prevention plays a critical role in lowering the incidence of colorectal cancer. By adopting effective strategies, individuals can significantly reduce their risk.
Healthy Diet
Maintaining a healthy diet is a powerful way to reduce the risk of colorectal cancer. Increasing fiber intake through fruits, vegetables, and whole grains promotes digestive health and decreases cancer risk. At the same time, limiting the consumption of red and processed meats is crucial, as studies have linked high intake to a 29% increased risk of colorectal cancer.38 Even small, consistent dietary changes can have a profound impact on preventing CRC development.
Healthy Lifestyle
Adopting healthy lifestyle habits is another essential component of colorectal cancer prevention. Engaging in regular physical activity, such as 150 minutes of moderate exercise or 75 minutes of vigorous exercise each week, helps maintain a healthy weight and lowers cancer risk.39 Similarly, reducing alcohol intake is vital, as excessive consumption has been associated with a higher likelihood of developing colorectal cancer.40 Implementing these small but meaningful changes into daily routines can lead to significant long-term health benefits.
Genetic Testing for Colorectal Cancer
For individuals with a family history of colorectal cancer, genetic testing is a critical tool for identifying inherited conditions like Lynch syndrome or familial adenomatous polyposis (FAP), which greatly elevate cancer risk. Understanding these genetic predispositions enables early and frequent screenings, offering opportunities to detect and address cancer before it develops. Proactive genetic testing empowers individuals and families to manage their health more effectively.41
Colorectal Cancer Screening
Regular colorectal cancer screenings are essential for early detection and prevention. The American Cancer Society advises that individuals at average risk begin screening at age 45. Screening options include stool-based tests and visual exams such as colonoscopies. These methods not only detect but also allow for the removal of precancerous polyps, helping to prevent cancer from developing. Early detection through screening dramatically improves treatment outcomes.37
Colorectal Cancer Screening
Early detection of colon cancer can significantly decrease the mortality rate and increase the 5 year survival probability of patients.1 The 5-year relative survival rate for stage I colon cancer in the US is about 92%. The five year relative survival rate decreases to 65% for stage IIB CRC.2 Additionally, patients usually do not experience any symptoms during early stages of CRC and therefore implementing routine screening for CRC is very important. Since the implementation of CRC efficient screening methods in the United States the incidence and mortality of colorectal cancer has decreased significantly.3 With screening, pre-cancerous polyps can be removed and the development of CRC can be prevented.4
The US Preventive Services Task Force strongly recommends individuals aged between 45-75 to get regularly tested for CRC. People with increased risk of CRC due to family history or certain conditions or diseases are recommended to start screening earlier.5 Currently colonoscopy, a direct visualization test, is the most commonly used screening technique of CRC in the US.6 There are two other visualization tests used, virtual colonoscopy and sigmoidoscopy. All three tests are invasive and involve pumping air into the colon.7
Stool tests for CRC are acceptable worldwide. Polyps and colorectal cancer can bleed. Guaiac fecal occult blood test (gFOBT) and Fecal immunochemical test (FIT or iFOBT) can detect the smallest amount of blood in stool.10 Multitarget stool DNA testing (Cologuard) is a FDA approved stool based test that detects hemoglobin, along with certain DNA biomarkers.11
Innovative Research in Colorectal Cancer Detection
Biomarkers from Blood
Advancements in colorectal cancer research are transforming CRC diagnostics and treatment. Currently there are two blood based tests that are FDA approved for CRC screening. Epi proColon 2.0 is approved for screening adults ages 50 years and over. This test detects methylated SEPT9, a molecular biomarker shed by colorectal cancer cells. Shield is approved for screening adults 45 and older. Shield analyses plasma DNA for presence of harmful gene variants and other changes.
Biomarkers from Stool
Stool tests are a non-invasive, safe, cost-effective, and convenient screening method for colorectal cancer (CRC). Growing evidence highlights the effectiveness of fecal biomarkers in CRC screening. Numerous potential stool-based CRC biomarkers are being identified and studied, including proteins, DNA mutations, epigenetics markers, microbes, and volatile organic compounds. These biomarkers are low-risk and hold great promise for transforming CRC screening and early diagnostic testing12.
The diagram below is adopted from an article written by Quan Ding et al.12 and summarizes some of the different stool biomarkers that have been associated with CRC.

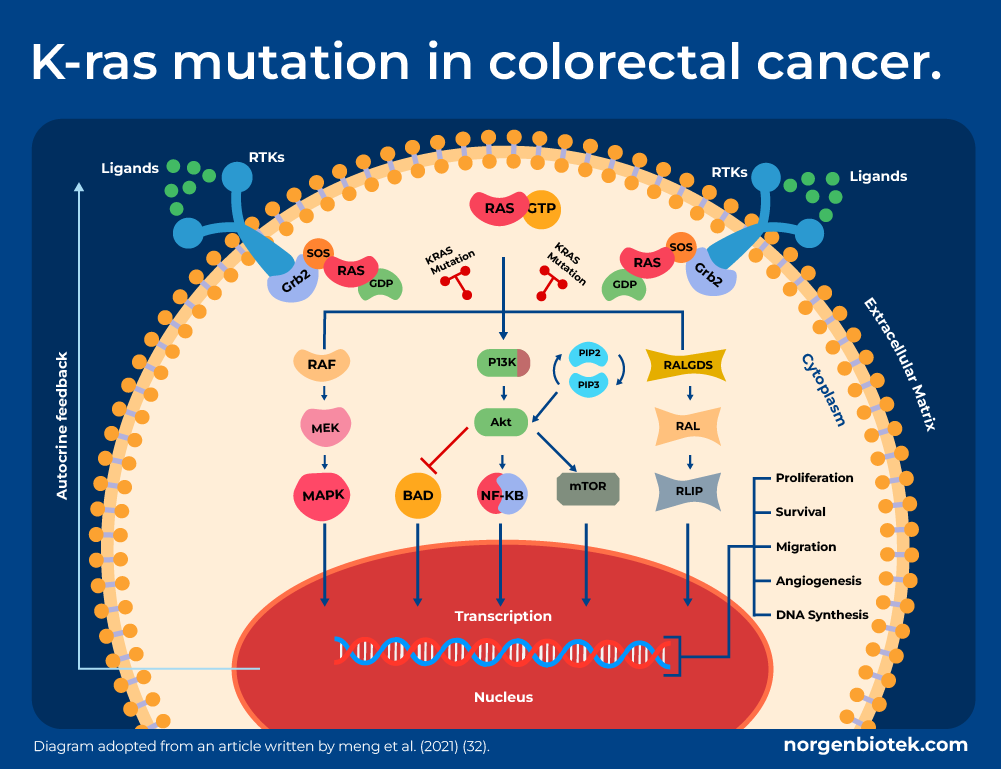
Stool DNA Biomarkers
Some of the most studied and common CRC biomarkers include mutations in the DNA. For example, mutated KRAS genes can result in uncontrollable cell growth and proliferation, which can lead to cancer. KRAS mutation is present in 40% of CRCs. Mutations in the Wnt signalling pathway can also be used as CRC biomarkers. The Wnt signaling pathway regulates the production of new cells to replace the continuous loss of cells, which is important in maintenance of intestine function. Mutations in this pathway lead to dysregulation of cell growth and division, which may progress to cancer. Mutations in this pathway are found in over 90% of CRC patients. Adenomatous polyposis coli (APC) is the most commonly mutated gene within this pathway.20
Stool RNA Biomarkers
Fecal microRNAs (miRNAs) show great promise as non-invasive diagnostic and screening biomarkers with significant clinical potential. These miRNAs remain stable and detectable in stool samples due to their packaging in exosomes, which protect them from degradation. Notably, fecal miRNA detection typically requires only 1 gram of stool, making the process highly practical for clinical applications. Emerging studies have linked specific miRNAs to colorectal cancer (CRC). For example, Ahmed et al. identified significant differences in miRNA expression in the feces of CRC patients. The study reported increased expression of miR-21, miR-106a, miR-96, miR-203, miR-20a, miR-326, and miR-92, alongside decreased levels of miR-320, miR-126, miR-484-5p, miR-143, miR-145, miR-16, and miR-125b.15 These findings highlight the potential of fecal miRNAs as reliable biomarkers for CRC detection and monitoring.

Another interesting finding that has opened many possibilities for CRC screening is the ability of profiling small RNA in addition to fecal immunochemical tests (FIT).14 In a study published in the molecular cancer journal, Birkeland et. al, using Norgen Biotek's RNA stabilizing solution and stool total RNA purification kit, showed that it is possible to detect the human miRNome in FIT leftover samples across populations and the analysis of small RNA biomarkers can complement the FIT in large scale screening settings. Also detected miRNAs from leftover FIT samples exhibited differential abundances between CRC patients and healthy individuals.14
Stool Microbiome Biomarkers
Associative studies using metagenomic techniques have identified bacterial species that have been enriched in CRC. These bacteria can be used as biomarkers for disease screening, prediction and treatment response.13 The discovery of next-generation sequencing technology has allowed the exploration of microbiomes from sources like the human gut, enabling observation of taxonomic and metabolomic relationships between the microbiome and cancer.
Studies examining the association of colon cancer with the human gut microbiome have yielded varying results. However, all these studies show that microbiota associated with a plant-based diet tend to be the ones associated with a lower incidence of colon cancer. A plant-based diet skews microbiota to produce short-chain fatty acids (SCFA) such as acetate, proprionate, and butyrate which have been shown to be anti-inflammatory via induction of T-regulatory cells in colonic tissues.16
Stool Microbiome Biomarkers
Norgen Biotek is a leader in stool DNA/RNA preservation and isolation systems, designed for the precision needed for the biomarker research. Our advanced reagents effectively stabilize nucleic acids for extended durations, ensuring consistent and reliable results in cancer diagnostics and research. Independent studies have demonstrated that Norgen Biotek's stool preservative outperforms competitors in preserving gut microbiota from stool samples.17, 18 Additionally, the preservative supports metabolomic studies, including short-chain fatty acid (SCFA) analysis.19 Norgen Biotek's stool DNA, RNA and nucleotide isolation can overcome two of the most prominent issues with stool samples, presence of humic acid and DNA fragmentation, with their advanced technology. Hence, these kits isolate great quality DNA or RNA with high yield from stool samples.
Beyond preservation, Norgen Biotek offers comprehensive next-generation sequencing (NGS) services for small RNA, miRNA, and metagenomics applications. Each service is accompanied by a detailed, project-specific bioinformatics report, empowering researchers with actionable insights tailored to their study's goals.
Conclusion: A Path Forward
Colorectal cancer is a serious but preventable disease when caught early. Advances in diagnostics, including biomarker analysis and innovative products like those from Norgen Biotek, are paving the way for better outcomes. Prioritize screenings, adopt a healthy lifestyle, and stay informed to reduce the risk of developing CRC.
For diagnostic tools and solutions tailored to colorectal cancer research, visit Norgen Biotek.
FAQs About Colorectal Cancer
How does the removal of polyps help prevent colorectal cancer?
As polyps grow, they may accumulate genetic mutations that could lead to their progression to cancer. This process takes several years. Removal stops this process by physically eliminating the tissue at risk.
Who should be screened for colorectal cancer?
Screening is recommended starting at age 45 for most individuals, earlier for those at high risk. Consult with your doctor to determine if you need to start screening earlier.
What foods are linked to increased colorectal cancer risk?
Diets high in red or processed meats and low in fiber are linked to increased risk of CRC.
Are stool-based tests reliable?
Stool tests are effective for initial screening and detecting early signs of cancer.
Is colorectal cancer hereditary?
Colorectal cancer (CRC) can have a hereditary component, but not all cases are hereditary. Most colorectal cancers are sporadic, meaning they occur due to environmental factors, lifestyle, or age-related genetic changes without a family history. However, approximately 5-10% of colorectal cancer cases are hereditary, resulting from inherited genetic mutations.